The kidneys are two bean-shaped organs. They are located below the rib cage on each side of your body. Most people without juvenile kidney disease are born with two functioning kidneys, but only need one to live a normal life. The kidneys filter ½ cup of blood every minute, removing waste and water. The water and fluid (urine) flow through two thin muscle tubes, called ureters to the bladder. Urine is stored in the bladder until it is ultimately released from the body. The combination of the kidneys, ureters, and bladder make up the urinary system. Key functions of the kidney include:
- Remove waste and extra fluid from the body
- Remove excess acid produced from the body cells and digested food
- Maintain a healthy balance of electrolytes and fluid—including sodium, potassium, calcium, and phosphorus
- Make hormones responsible for: control of blood pressure, making red blood cells for oxygen and energy and preserving bone strength
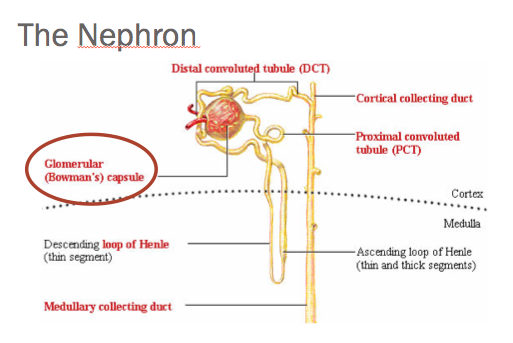
Each kidney is composed of over one million functioning cells called—nephrons. Each nephron is composed of two parts—a filter called a glomerulus and a tubule.
When the kidneys are damaged, this can lead to symptoms of swelling, shortness of breath, increased sleepiness and fatigue, bone pain, nausea, vomiting, and poor appetite with weight loss.
Damage to the kidney can be acute (sudden) or chronic (lasting longer than 3 months).
Acute damage can result from not enough blood flow to the kidney, direct damage to the kidney or urine backing up in the urinary system (otherwise known as obstruction).
Common causes of acute injury include:
- Trauma
- Infection
- Dehydration
- Enlarged prostate
- Liver/heart failure
- Medication (including antibiotics and anti-inflammatory drug)
- Auto-immune disease
- Causes of chronic kidney disease (greater than 3 months) include:
- Diabetes Mellitus—Type I and Type 2
- Hypertension (high blood pressure)
- Immune diseases—genetic diseases, vascular diseases
- Viral disease—HIV, Hepatitis B, C
- Urinary tract infections—recurrent
- Drugs
- Blockages in the tubule
- Cystic kidney disease
Facts about Chronic Kidney Disease:
- Prevalence: 14% of the country is afflicted with the diagnosis of kidney disease—15 million Americans
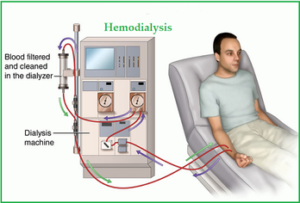
- Over 660,000 are currently living with the diagnosis of End Stage Renal Disease. Of these approximately 467,000 individuals are on a life-saving mechanism called dialysis—renal replacement therapy. Of those, greater than 60,000 are doing dialysis at home.
- 100,000 people a year are waiting for a kidney transplant. Currently, 17,000 individuals a year receive a transplant (either living or deceased).
- The prevalence of kidney disease increases every decade of life, from 6.6% between the ages of 20-39 to over 33% by the age of 60+
- Fewer than 10% of the population is aware they have kidney disease. Only 50% of people with stage 4 kidney disease (see below) are aware of their diagnosis.
- Only 30% of patients with a diagnosis of kidney disease have ever seen a Nephrologist (kidney doctor).
- Less than 50% of people with a diagnosis of kidney disease stage 3b or worse (see below) have seen a kidney doctor at least once.
- Patients with kidney disease are hospitalized at 4 times a higher rate than patients at a similar age without the diagnosis of kidney disease
- Patients with kidney disease diagnosis are re-admitted into the hospital within 30 days at 1.5 times higher rate than those at a similar age without kidney disease
- Patients with kidney disease have 2.5 times higher mortality (death rates) than those patients without kidney disease at a similar age. For patients between the ages of 60-74, the mortality rate is 4 times higher
- African Americans are over 3 times more likely to develop kidney disease versus Caucasians
- Women have a higher prevalence of kidney disease versus men, but men have higher mortality (death) rate at every stage (see below).
- Mortality rate (death rate) because of cardiovascular (heart complications) is 3 times higher for patients with kidney disease versus aged match patients without kidney disease
- Every stage of kidney disease (see below) is associated with much higher risk of dying from cardiovascular complications (congestive heart failure, coronary artery disease, arrhythmias) vs non- kidney disease individuals at the same age
- The two main risk factors for chronic kidney disease are diabetes (as a primary cause–39.4% of all kidney disease patients) and hypertension (as the primary cause –high blood pressure –32.1%)
- Average yearly Medicare cost–$50 billion dollars—20% of all Medicare expenses for all kidney disease patients
- The average cost of a dialysis patient–$75,000 to $110,000/year—more than 10 times the average cost of a non-kidney disease patient in a given year
- Dialysis patients are 1% of the Medicare population, yet 8% of the cost.
- Cost of care increases every stage of kidney disease (see below) exponentially.
Stages of Kidney Disease:
(eGFR—glomerular filtration—measure of blood flow/minute flowing through kidney)
Average for male—110-120ml/min; for women 100-110 ml/min)
| Gfr | sxs | |
|---|---|---|
| Stage 1: minimal loss of function | 90-120ml/min | none |
| Stage 2: mild loss of function | 60-89 | none |
| Stage 3a: moderate | 45-59 | none |
| Stage3b: moderate/severe | 31-44 | anemia, bone pain, Malaise, neuropathy, Decreased mentation |
| Stage4: severe | 16-30 | swelling in legs, anemia, decreased appetite, Nausea, increased blood pressure, Fatigue, abnormalities of calcium, Phosphorus, vitamin d |
| Stage5: ESRD | 0-15 | all of the symptoms in stage 4 + Shortness of breath, swelling of legs, arms, face, back, abnormalities of potassium weight loss, severe difficulties with mentation. |
| What it Measures | How it’s Performed | What Results Mean | |
|---|---|---|---|
| Albuminuria-to-Creatinine Ratio (ACR) | Measures a type of protein called albumin in the urine | Spot urine sample test | 30 mg/gm or less = normal
Higher than 30 mg/gm = a possible sign of kidney disease. |
| Blood pressure | Presence of high blood pressure (hypertension), a leading cause of kidney disease | In the doctor’s office with an inflatable cuff, pressure guage and stethoscope | High blood pressure may indicate elevated risk of CKD and Requires further diagnostic testing |
| Serum creatinine | Levels of Creatinine, as waste product from normal muscle use | Blood analysis | Serum creatinine results of greater than 1.2 for women or greater than 1.4 for men = early sign that kidneys are not working properly |
What makes us more susceptible to kidney damage:
- Older age
- Family history of kidney disease
- Smaller kidney mass/size
- Lower birth weight
- Low income, education
- Racial/ethnic disparities
Causes of chronic kidney disease (see above):
Progression Factors:
- Higher level of protein in the urine
- Poor blood pressure control (goal blood pressure should be at least 140/90, but in most cases less than 130/80
- Poor sugar/diabetes control
- Poor cholesterol control
- Smoking
- Poor weight control
Quick facts:
-
-
- Diabetes: affects the glomerulus –leading to protein in the urine (causing leg and ankle swelling). Kidney disease will occur and progress rapidly with poor sugar control, blood pressure control and family history.
- Type I diabetics will begin to see affects of kidney disease up to 5 years after diagnosis. With progression to severe kidney disease anywhere between 10-30 years later, depending on the level of control.
- Type II diabetics have a similar timeline, but occurring with diagnosis later in life.
- Screening includes serial urine protein measurements and treatment with ace-I or angiotensin blockers. Often will need water pills (diuretics) for swelling control
- Hypertension affects the blood vessels and tubules in the kidney, preventing the elimination of fluid and waste. The buildup of fluid and waste causes more damage to the vessels, causing further waste buildup. This vicious cycle leads to progressive kidney failure. To prevent progression: aggressive blood pressure control, compliance with medications, exercise and LOW SALT DIET.
- Diseases that affect the glomerulus (Glomerular Diseases—Lupus, IgA, minimal change, HIV, Vascular diseases etc.) cause damage to the glomerulus resulting in protein and blood in the urine with high blood pressure:Treatment includes ace-I or angiotensin blockers for kidney protection/reduce protein in urine and blood pressure controlSteroids for diseases attacking the immune systemWater pill (diuretics) to help prevent swelling.
- Diabetes: affects the glomerulus –leading to protein in the urine (causing leg and ankle swelling). Kidney disease will occur and progress rapidly with poor sugar control, blood pressure control and family history.
-
To conclude kidney disease is a severe problem, with serious health and financial consequences. Early diagnosis and regular follow up and preventative treatment will greatly reduce the progression of this disease and the burden it places on patients, family members, the health care system and society.
